Tachycardia:
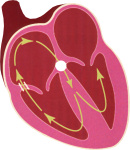
Normally one is not aware of one’s own heart beat. When one runs to catch the bus one is aware of it beating away, but assumes it to be a normal occurrence and pays no particular attention. However if the heart starts beating fast when you would least expect it, you begin to notice it. Tachycardias can be divided into those originating in the atria (so called Supraventricular tachycardias –SVT) or those coming from the ventricles (Ventricular tachycardias). In either case, an abnormal electric circuit spreads around the heart in either a random or defined manner. Symptoms are usually experienced as palpitations. In certain people the circulation becomes less effective fast heart rates and can cause dizziness, breathlessness, and sometimes collapse.
Fit-bit Arrhythmia
With the advent of more heart rate trackable devices, people are recording abnormal heart rates. They are generally sporty types who will notice these heart rate changes where the heart rhythm can become too slow, too fast, or irregular. It is important not to be dismissive of such recordings, although in my experience, heart rate fluctuations are usually benign, especially if the person has no associated symptoms of fatigue, palpitations or dizziness. Most people are usually reassured, but we may need to check things out, especially if there are associated symptoms.
Treatment of Arrhythmia
Depending on the type of arrhythmia, the treatments will vary. For infrequent benign disturbances, no treatment is necessary. For certain arrhythmias, a pill can sometimes be prescribed to abort an attack (so called “pill-in-a-pocket”). For more regular rhythm disturbances, prophylactic daily medication is often prescribed. In certain cases, if medication is ineffective or causes side effects, then more curative treatment by radiofrequency ablation can be used to “burn away” an abnormal electrical pathway.
 Supraventricular Tachycardias: Supraventricular Tachycardias:
These occur when an abnormal electrical circuit starts in the atrium. Sometimes this follows a defined electrical pathway in a circus manner causing a regular fast rhythm. This can cause sudden onset of a fast regular palpitations. Attacks can last a variable length of time and stop spontaneously. One type is called Atrioventricular Re-entrant Tachycardia (AVNRT) and results due an extra piece of wiring in the atrioventricular node. Another type is called Wolf Parkinson White Syndrome, and occurs when an extra bit of wiring connects the atrium to the ventricle to cause an abnormal circuit. Treatment in the first place usually involves daily medication with anti-arrhythmic drugs to prevent attacks. Increasingly, patients with infrequent episodes are given medication to take to abort an attack (so called “pill in a pocket”). For those patients who are resistant to the effects of medication, or who develop side effects, then potentially curative treatment can be achieved by radiofrequency ablation (see later). Atrial fibrillation is a particularly common tachycardia and is considered separately in the next section.
Ventricular Tachyarrhythmia (VT):
This can occur in many situations. Although benign types of this disturbance can occur, more dangerous types of it need to be excluded. Often it is a result of scarring within the heart muscle (myocardium), that can occur after a myocardial infarction or damage after viral infections affecting the heart (myocarditis). Benign versions of VT include “right ventricular outflow tract tachycardia”, and this can be treated with either drugs or ablation. For more dangerous types of ventricular arrhythmia, either drugs, ablation or a defibrillator (ICD) should be considered.
A particular type of VT that can run in families or be induced by certain medication called Long QT Syndrome. This may be inherited from family members who might have collapsed or passed away suddenly. It is often picked up in normal people who have had a routine ECG where the QT interval after the main electrical spike is prolonged (>450 msec in men and >470 msec in women). In the absence of symptoms, nothing necessarily needs to be done if there is only mild prolongation. However, the main concern is certain medications especially pain killers, anaesthetic agents, and most commonly antibiotics (especially Clarithromycin). In anyone with known QT prolongation being prescribed any medication, the list of drugs that can aggravate this, needs to be scrutinised. It is worth such patients having a list to compare (see reference: https://crediblemeds.org/pdftemp/pdf/DrugsToAvoidList.pdf. With significant QT prolongation and certainly with associated symptoms (palpitations, dizziness or collapse, urgent assessment is recommended. In certain such patients either medication or a defibrillator may be required.
Implantable Cardiac Defibrillator (ICD):
This is a device a little like a pacemaker that is implanted under the skin. Wires pass from device to the heart via the veins under the collar bone. It has the function of recognising any significant dangerous ventricular arrhythmias, and treating them automatically either by pacing the heart back to normal, or electrically shocking the heart back to normal. Most patients that require these devices are those who have had a heart attack and left with a poorly functioning heart (so called heart failure). In some cases it is patients who have structural abnormalities of the heart (cardiomyopathy) who are at risk of arrhythmias who warrant the device. Occasionally, patients with a family history of collapses who are thought to have genetically acquired the same condition (e.g Long QT syndrome, Brugada syndrome) may warrant the device.
Prior to any consideration of an ICD implant, a series of tests are undertaken to risk assess the patient. If the risk is considered significant, then implantation is considered appropriate.
Once the device is implanted (usually under local anaesthetic as a day case), it is tested to ensure that it can recognise abnormalities. Subsequently, the device is checked on a regular basis to make sure it continues to recognise abnormalities. Roughly every 5 or so years, the battery of the device will need to be changed, which is a far less cumbersome procedure. |